Chiropractic Patients Less Likely to Suffer Drug Reactions
Most people experience back pain, and many of these patients use drugs for pain relief. A 2014 study1 found that of older adults with chronic back pain, 72% of them were using some kind of analgesic to help cope with the pain. Another study2 found that 32% of back pain patients in their analysis were using prescribed opiates for relief.
It’s unfortunate that so many patients depend on drugs for musculoskeletal aches and pains, especially when chiropractic is an effective and safe way to not only relieve pain, but also prevent future pain episodes.
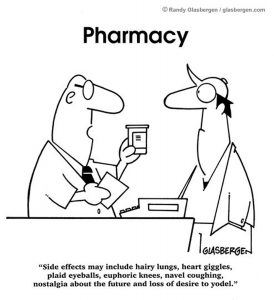
Now a new study3 shows that chiropractic also is linked to a lower risk of adverse drug reactions in patients with back pain. In this study, the authors looked at the medical records of over 19,000 adults in New Hampshire who had at least two doctor visits for back pain. 9.810 of these patients used chiropractic care; 9,343 patients used regular medical care. The researchers analyzed the number of adverse drug effects (ADEs) experienced by the two groups.
The authors found:
- Younger patients were more likely to use chiropractic care.
- Non-chiropractic patients tended to have more health problems, in general, when compared to those who used chiropractic.
- Chiropractic patients experienced 51% fewer adverse drug reactions (.4% vs .9%) compared to medical patients.
- 15 non-chiropractic patients were diagnosed with drug withdrawal, while zero chiropractic patients had drug withdrawal.
This study had some limitations, as the study data didn’t included details about the types of drugs the patients were using or how frequently they were using medications. But the authors conclude that the “utilization of chiropractic care may be associated with reduced risk of ADEs; however, no causal relationship has been established.”
Another study by the same group of researchers found that chiropractic patients were 55% less likely to be prescribed opiates for their pain and had lower health care bills.
With the opiate epidemic in the US, it’s critical that we find non-opiate approaches to back pain treatment. Chiropractic is about restoring health without the use of drugs. By helping the body heal naturally, chiropractic can help you stay well and help you avoid unnecessary adverse drug reactions, too!
- Enthoven WT, Scheele J, Bierma-Zeinstra SM, Bueving HJ, Bohnen AM, Peul WC, van Tulder MW, Berger MY, Koes BW, Luijsterburg PA. Analgesic use in older adults with back pain: the BACE study. Pain Medicine 2014 Oct;15(10):1704-14. Doi: 10.1111/pme.12515.
- Ashworth J, Green DJ, Dunn KM, Jordan KP. Opioid use among low back pain patients in primary care: Is opioid prescription associated with disability at 6-month follow-up? Pain. 2013 Jul;154(7):1038-44. doi: 10.1016/j.pain.2013.03.011.
- Whedon JM, Toler AWJ, Goehl JM, Kazal LA. Association Between Utilization of Chiropractic Services for Treatment of Low Back Pain and Risk of Adverse Drug Events. Journal of Manipulative & Physiological Therapeutics 2018 May 26. pii: S0161-4754(17)30136-7. doi: 10.1016/j.jmpt.2018.01.004.


 A new study just published in the Journal of the American Medical Association finds that opioids are not an effective solution for chronic pain.
A new study just published in the Journal of the American Medical Association finds that opioids are not an effective solution for chronic pain. With the huge rise in the use of antibiotics over the past 70 years, some pathogens are now becoming resistant to the drugs that once easily eradicated the illnesses these pathogens cause. People who become infected with one of these drug-resistant organisms are at increased risk for longer, more costly hospital stays and are more likely to die from their infection.
With the huge rise in the use of antibiotics over the past 70 years, some pathogens are now becoming resistant to the drugs that once easily eradicated the illnesses these pathogens cause. People who become infected with one of these drug-resistant organisms are at increased risk for longer, more costly hospital stays and are more likely to die from their infection.