
In this age of mobile devices and smartphones, more and more patients are being diagnosed with neck pain associated with looking down at a screen.
Studies have shown that young people are at increased risk of back and neck pain due to overuse of devices. Now, a new condition, dubbed “text neck,” is being found in smartphone-users of all ages, resulting in serious stiffness, strain, and pain in the neck muscles and cervical spine.Americans send an average of around 2.19 trillion text messages every year, meaning that text neck has the potential of afflicting millions of people.
The condition is relatively new, and as Forbes reports in their article, How Texting Can Give You a Permanent Pain in the Neck, “It takes time…for a new condition to spread throughout the medical community. Some doctors who have never heard of text neck don’t think to ask patients with neck pain about their phone or computer habits.”
However, investigators of worker’s compensation claims are at the point that they look into the phone records of claimants with neck pain, and sometimes use their history of text messaging to get their compensation cases dismissed, attributing the neck pain to personal screen time rather than work.
There is no denying that a great number of people consider smartphones to be indispensable. And this overuse is causing what could be an epidemic of health problems into the future. A study published in the journal Applied Psychophysiology and Biofeedback found that an overwhelming majority of 83% of participants reported some hand and neck pain during texting. Researchers in this study also found that people sending texts displayed other classic signs of tension, such as increased heart rates and holding their breath. Even when they said they were relaxed, they had signs of tension.
If you text or play games on your smartphone, you know that it is easy to get into the habit of holding your head forward-and-down while typing on it. Another study conducted at the Center for Musculoskeletal Research found that 90% of people flexed their necks while texting, defined as bending the neck forward over 10 degrees past neutral alignment. In this study, it was discovered that the more texting that participants did, the worse their risk of neck or shoulder pain.
Especially susceptible to text neck are those of us who not only spend some of our leisure time on smartphones, but also spend much of our working time sitting at computers. All these hours spent in a flexed posture can add up to 30 pounds of extra weight on the upper vertebrae, straining the trapezius muscles and pulling the spine out of alignment over time.
Researchers are also finding that people over age 50 are more at risk of developing text neck. According to physical therapist Rob Worth, in an interview with Forbes, “People in their 50s and 60s have less tissue tolerance. Overuse injuries (like text neck) don’t heal as quickly.”
However, Worth said that young people are also at risk of permanent problems from text neck. He suggested that the stooped posture while typing on phones may freeze the position of the spine’s alignment, and years down the road, we may see people who are permanently stooped because of it.
If you suspect you have text neck, talk to your health-care provider. Your chiropractor or physical therapist can help you determine if you’re suffering from this ailment. These experts can also help design a treatment plan to relieve pain and regain range of motion, as well as advise you about preventing future injury. The following tips, summarized from the Forbes article, may help you avoid the risks of text neck:
- Hold your phone at a proper reading angle, rather than looking down. Your phone should be held directly in front of your mouth, a few inches across from your chin. Your eyes should look down rather than having to bend your neck down. Your shoulders should feel relaxed while you’re typing.
- Use a text-dictation program if you have one. Hold the phone in front of your mouth.
- Set a timer and take breaks. Avoid prolonged phone use by taking regular breaks where you put your phone down and do something else.
- Build strength and range of motion. In your workout routine, include exercises and stretches that strengthen your neck, back extensors, rhomboids, and latissimus dorsi muscles.
- Drink water and maintain hydration.
- Use other forms of communication. Try calling your family and friends or seeing them in person to chat.
When you have a case of text neck, be sure to come in and get your adjustment from Dr. Oblander. Don’t allow your neck issues to create lingering problems for you!
References
Quilter D. How texting can give you a permanent pain in the neck. Forbes June 7, 2013. www.forbes.com.
Lin IM, Peper E. Psychophysicological patterns during cell phone text messaging: a preliminary study. Applied Psychophysiology and Biofeedback March 2009; 34(1): 53-57.
Gold JE, Griban JB, et al. Postures, typing strategies, and gender differences in mobile device usage: an observational study. Applied Ergonomics March 2012; 43(2): 408-412.
Peper E. Improve health with fun movements: practices you can do at home and at work. The Peper Perspective blog; February 2, 2013.
Written by: Kelly Johnson and revised by Marissa Luck
Article shared from www.chironexus.net
 Learning the risk factors of sciatica can help you minimize your risk of developing it. A recent study sheds light onto what makes you more likely to develop sciatica.
Learning the risk factors of sciatica can help you minimize your risk of developing it. A recent study sheds light onto what makes you more likely to develop sciatica.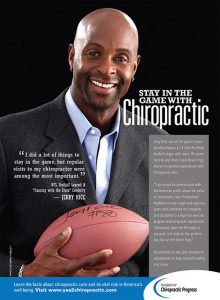
 In this age of mobile devices and smartphones, more and more patients are being diagnosed with neck pain associated with looking down at a screen.
In this age of mobile devices and smartphones, more and more patients are being diagnosed with neck pain associated with looking down at a screen.  Many studies have found that chiropractic care is a safe and effective treatment method when dealing with a number of spine-related issues. The American Chiropractic Association even lists a number of research studies on their website that show that it is a valuable treatment method for easing (and sometimes completely resolving) back pain, neck pain, headaches, and more.
Many studies have found that chiropractic care is a safe and effective treatment method when dealing with a number of spine-related issues. The American Chiropractic Association even lists a number of research studies on their website that show that it is a valuable treatment method for easing (and sometimes completely resolving) back pain, neck pain, headaches, and more. Countless studies have demonstrated that chiropractic care is a safe and effective way to treat musculoskeletal complaints like back pain, neck pain, or sciatica. Now a new study from Switzerland has looked at the relative benefits of chiropractic compared to medical care for the most common types of pain issues.
Countless studies have demonstrated that chiropractic care is a safe and effective way to treat musculoskeletal complaints like back pain, neck pain, or sciatica. Now a new study from Switzerland has looked at the relative benefits of chiropractic compared to medical care for the most common types of pain issues.



 When it comes to helping elite athletes prevent and recover from injuries—as well as achieve peak performance—chiropractic care can offer many advantages. That’s why large numbers of professional and college sports teams throughout the U.S. have turned to chiropractors over the past decade. The Philadelphia Phillies is one such team, and Dr. Michael Tancredi is one such chiropractor. As a Doctor of Chiropractic, a Certified Chiropractic Sports Physician, an Active Release Technique Instructor and Practitioner, and a certified athletic trainer, Dr. Tancredi clearly understands the valuable role that chiropractic care can play in keeping teams healthy and performing at their best.
When it comes to helping elite athletes prevent and recover from injuries—as well as achieve peak performance—chiropractic care can offer many advantages. That’s why large numbers of professional and college sports teams throughout the U.S. have turned to chiropractors over the past decade. The Philadelphia Phillies is one such team, and Dr. Michael Tancredi is one such chiropractor. As a Doctor of Chiropractic, a Certified Chiropractic Sports Physician, an Active Release Technique Instructor and Practitioner, and a certified athletic trainer, Dr. Tancredi clearly understands the valuable role that chiropractic care can play in keeping teams healthy and performing at their best.